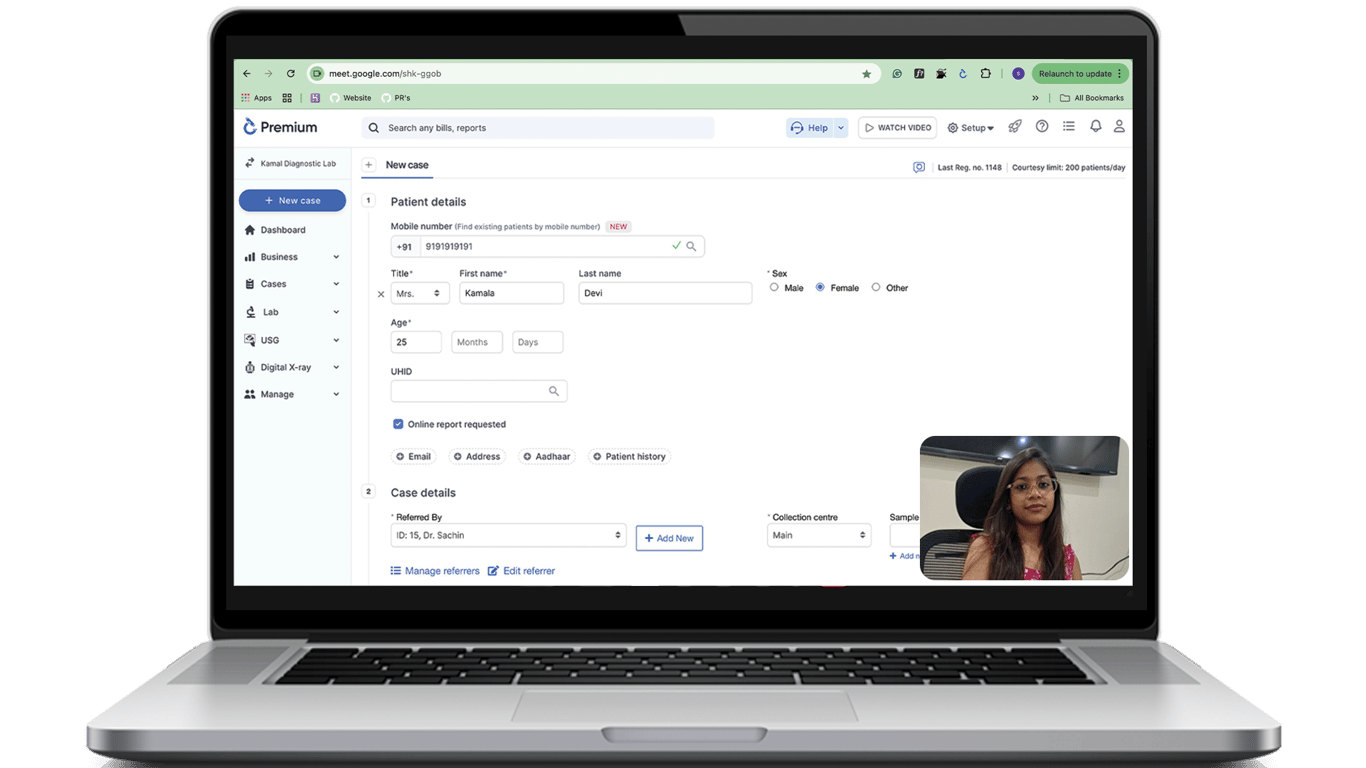
Join a free live demo now!
See all features live
Understand the benefits
Get your questions answered
No purchase pressure
What is Glucose-6-phosphate dehydrogenase ?
G6PD is an enzyme that plays a critical role in protecting red blood cells from oxidative stress. A deficiency in this enzyme can lead to the destruction of red blood cells, a condition known as hemolysis. G6PD deficiency is typically diagnosed through blood tests, and the results are essential for guiding treatment decisions, especially in patients who are at risk of hemolytic anemia.
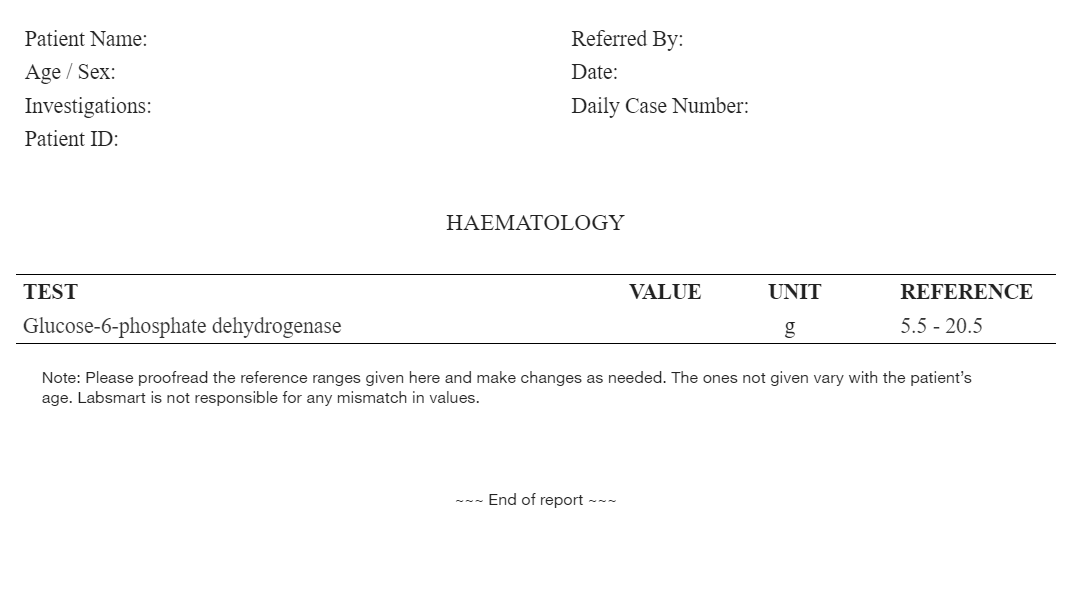
Glucose-6-phosphate dehydrogenase Report Format: Breakdown
Here’s what an ideal G6PD report format should include:
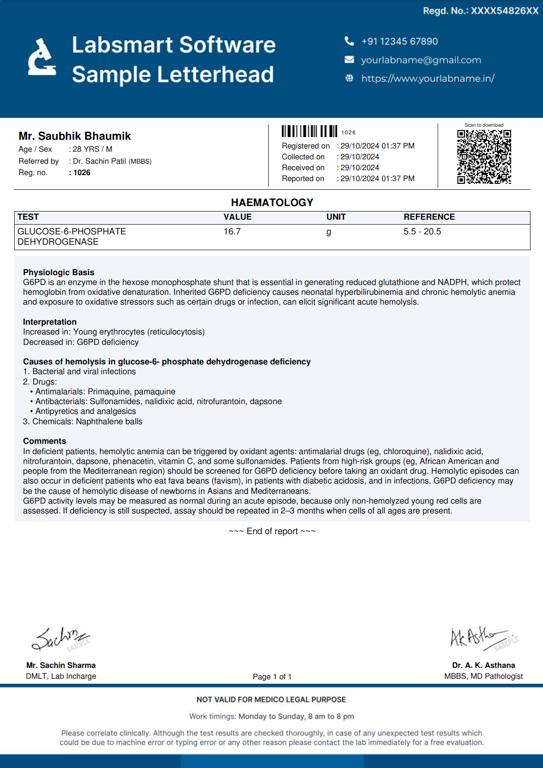
Header Information:
- Patient Details: Full name, Age, Gender, and ID.
- TAT information: Timestamp for both sample collection and report generation.
- Doctor's Information: Name of the referral doctor, if applicable.
Test Results Section:
-
Patient's results
As obvious as it is, a test report should definitely have the patient's test result.
-
Result's Unit
The unit of the test result must be mentioned correctly in the report. Glucose-6-phosphate dehydrogenase test is generally reported in “g”
-
Glucose-6-phosphate dehydrogenase Normal Value / Reference Range
The report must have the normal Glucose-6-phosphate dehydrogenase range. It can differ slightly based on the reagents used by the lab and other internal factors, but common Glucose-6-phosphate dehydrogenase ranges are:
For any gender, 0 to 100 year of age: 5.5 - 20.5
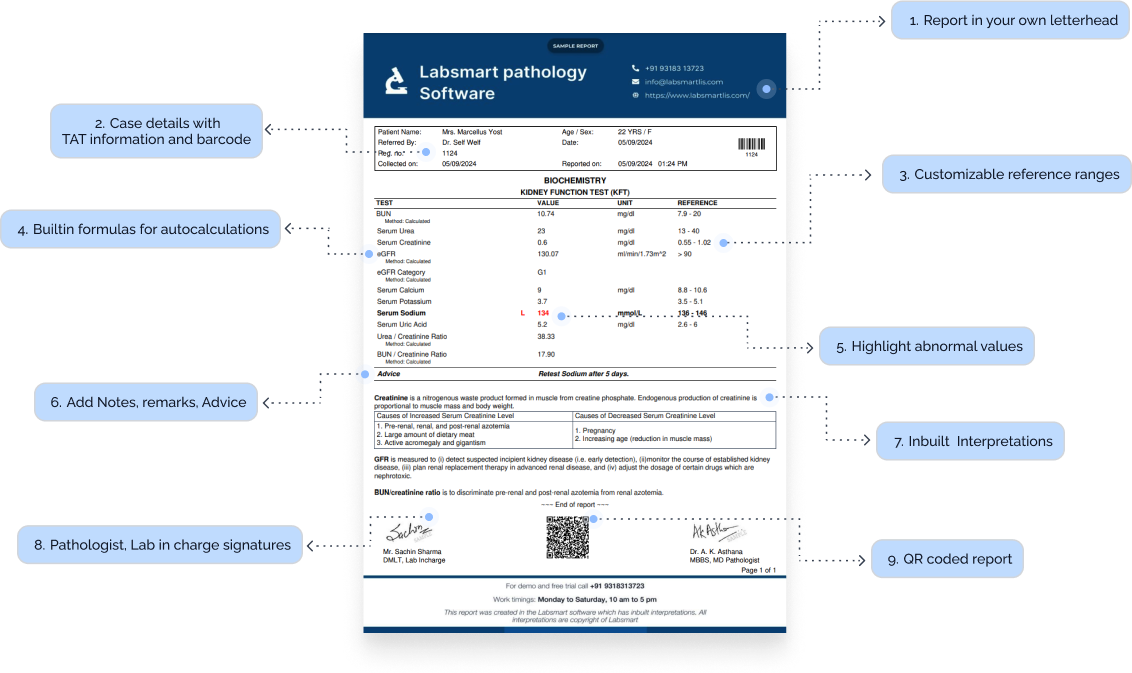
Interpretations
Nowadays, most labs prefer to add interpretations to the reports, making the report more patient-friendly. Labsmart software has interpretations of all routine test pre-filled in the software.
Footer Section:
-
Certifications:
Display any relevant accreditations (e.g., NABL, ISO), adding to your lab's credibility.
-
Pathologist and technician signature:
It's mandatory to add a Pathologist and technician signature to the report.
G6PD Interpretation
In Labsmart software, this is the inbuilt interpretation for Glucose-6-phosphate dehydrogenase
Importance of adding interpretation to reports:
It's very helpful to add interpretation in reports as it makes the reports more patient friendly and also helpful to doctors in some cases. Moreover, presently most labs prefer providing reports with interpretation. Thus, adding interpretation to report will help your lab stay at par with other competitor labs.
Labsmart Pathology Reporting Software
(With Interpretation and auto calculations)
- Billing
- Reports with Interpretation
- Auto calculation where needed
- Check daily business
- WhatsApp reports
1.5 Crore+
Reports printed & delivered online
1250+
Labs Active
10+
Countries
G6PD MS Word format
Download the Ms word editable Glucose-6-phosphate dehydrogenase report format for offline reporting.
Download word format